What is an STI?
Sexually transmitted infections (STIs) are, as you would imagine, infections transmitted via sexual contact. Often passed on unwittingly, they can often exist in the body for a long time without causing any symptoms but remaining live to transmission. There are more than 30 infections, with the most common ones including chlamydia, gonorrhoea, syphilis and trichomoniasis.
Fun fact: Over half a million people are diagnosed with an STI every year in the UK.
How do I get an STI?
Let’s start from the top – literally. STIs can be spread from any form of sex, including, and especially, oral.
We advise condom use from the start of any sexual contact as infections spread through bodily fluids: that’s saliva, semen, vaginal fluids and blood. Others can spread via skin-to-skin contact, for example, warts and herpes.
Concerned? Find more info on specific infections here.
How do I know if I have an STI?
Many common STIs can have no symptoms whatsoever. Consequently, people can be infected for long periods at a time without a clue, so please don’t be complacent, even if you are feeling absolutely fine.
Others infections cause symptoms such as pelvic pain, genital itching, discharge, urinary discomfort, unscheduled menstrual bleeding, amongst others.
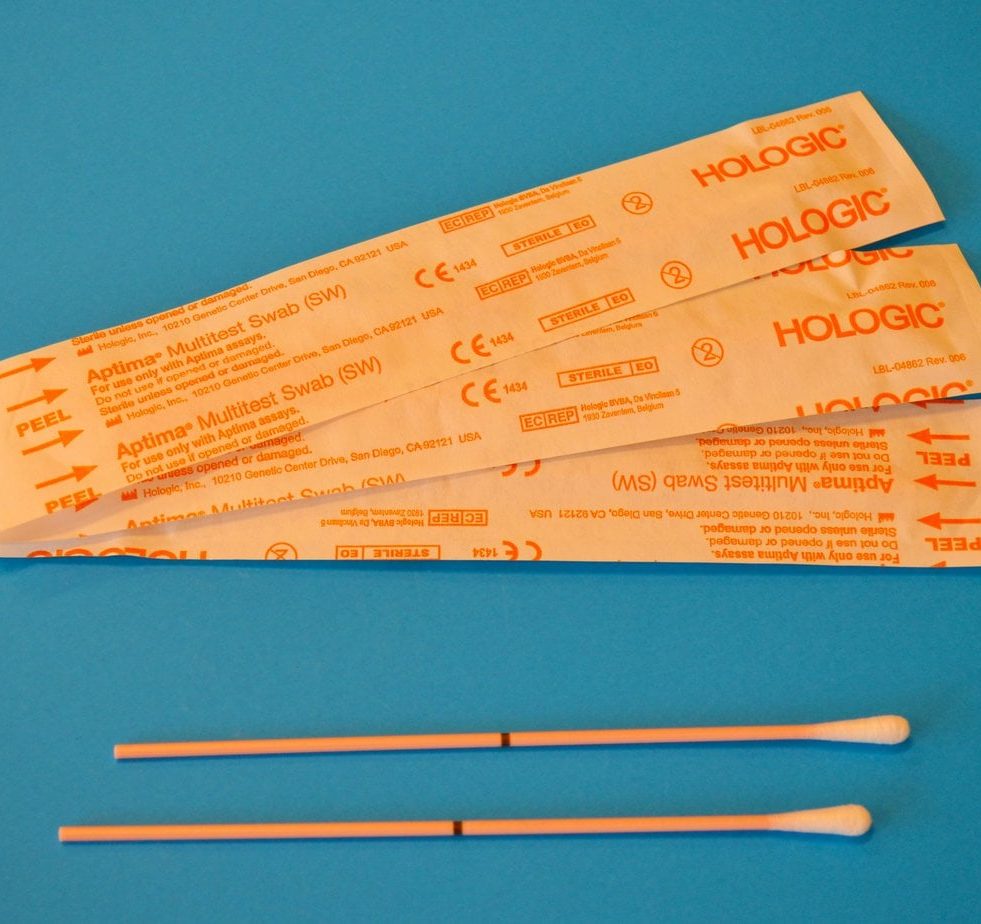
To diagnose an STI, you need to be seen by a healthcare specialist; this can be at your GP surgery, sexual health clinic or gynaecologist. Testing will vary depending on your symptoms and sexual history.
Feeling nervous?
These investigations aren’t necessarily as invasive or scary as they might sound. From peeing into a pot to blood tests and examinations with swab testing, if there are tests you are uncomfortable taking, you won’t be forced into anything.
Sexual health clinics are happy to discuss your relationship history and ask about any symptoms you may have. These clinics are all anonymous and completely non-judgemental.
And, as our co-founder and gynaecology doctor, Dr Sarah Welsh says, “You will never surprise a sexual health worker. Believe me.”
Whatever your question, there isn’t any good reason not to ask when it comes to your health. So, whether you want to know ‘Can you get chlamydia from a lap dance, kissing, or toilet seats?’, ‘Can you have more than one STI at a time?’ or ‘Can I catch an STI again if I’ve already had it before?’ make sure you ask. A little embarrassment is far easier to get over than an STD left to develop into something far more serious.
What happens if I don’t get treated?
Most STIs are easily treatable and honestly, the sooner you get treatment, the better, as this can prevent any long-term damage. For example, if it’s chlamydia, you may only require one dose of antibiotics, and you’re all set! Long-term infection can cause chronic pain, cervical cancer, pregnancy risks, internal scarring and infertility. Why wait when you could sort that STI out in no time at all?
How do I protect myself and my partners?
Protect yourself against getting infected in the first place and use a condom and other barrier methods, such a dental dams and gloves.
Barrier protection helps mitigate the risk of STIs in nearly every case and they are essential in practising safe sex.
Here are our top HANX tips for staying safe and keeping those STIs at bay:
- Use condoms and other barrier methods at the start of all sexual relationships purely for STI protection (not even considering their other uses, such as prevention of pregnancy, if that’s relevant to your situation).
- Ensure you have regular STI testing if you have new sexual partners. Whatever they tell you about their sexual health status, you need to take control of your own body and ensure your own wellness.
- If you have any unusual symptoms, including genital itching, unusual discharge or urinary symptoms, be sure to have an STI check. As many STIs have no symptoms or signs, seek regular check-ups anyway, as with long-term consequences including the possibility of infertility and chronic pain, you can’t afford to be complacent.
Make sure to protect your sexual future, stay informed and play safe.
Discover HANX sustainable sexual wellness products here.

Written by the Killing Kittens team.